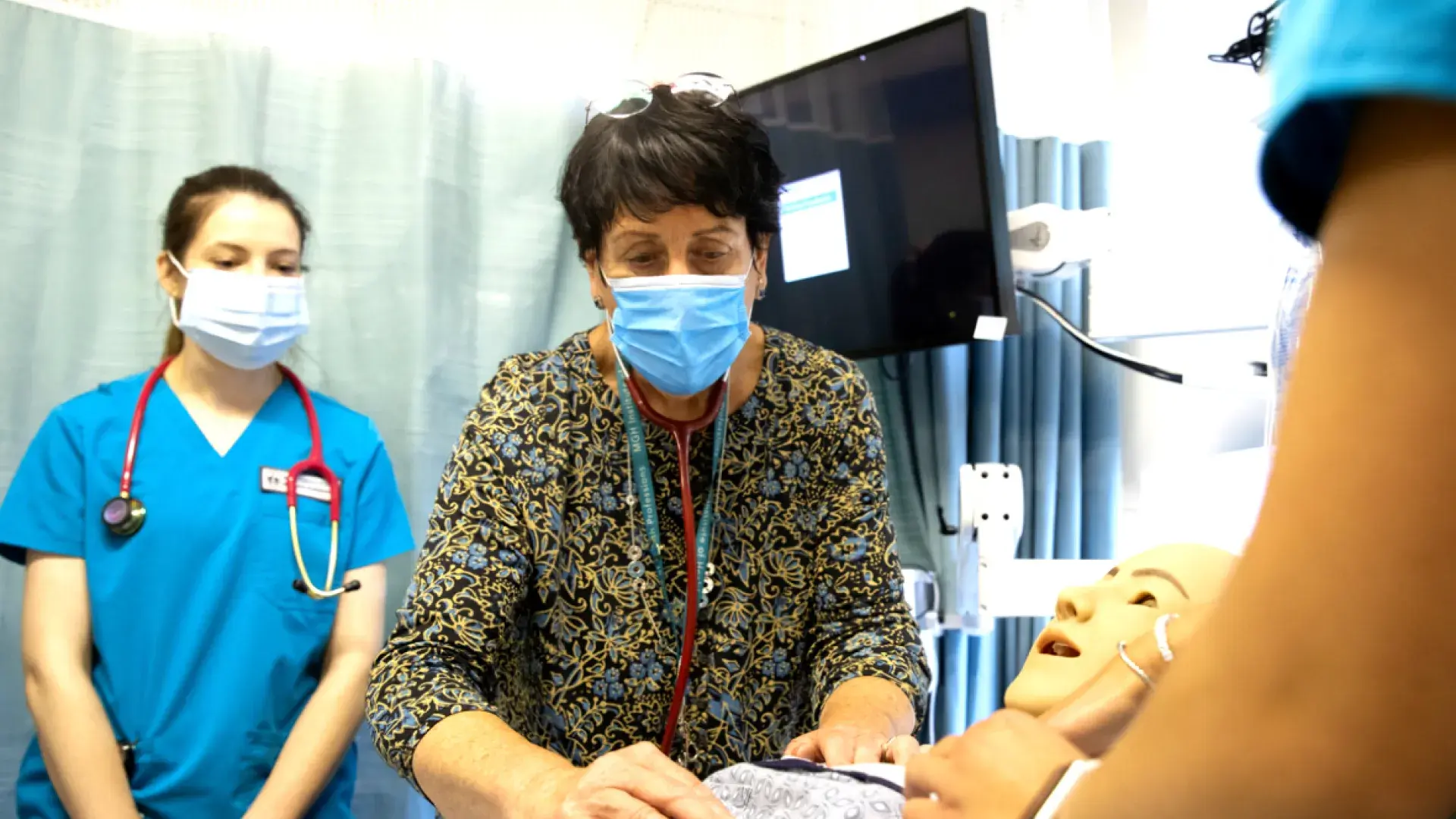
Teach tomorrow's healthcare leaders.
Preceptors provide the bridge from theoretical concepts to real-world practice and prepare students to offer high-quality, compassionate healthcare. Being a preceptor is a way to make your own contribution to the future of this essential profession.
If you are interested in becoming a School of Nursing RN or Advanced Practice preceptor or for more information, please contact us.
Why become a Preceptor?
Why do busy healthcare professionals become preceptors? They often share that they remember their own clinical experiences and how they shaped them into the providers they are today. Being a preceptor is a way to give back and make your own contributions to the future of this essential profession.
The MGH Institute of Health Professions offers special reduced tuition benefits to all employees of Mass General Brigham, including all its members and affiliates. Through the IHP Tuition Reduction and Incentive Plan, preceptors have access to a variety of benefits to support your ongoing professional development and accelerate your career growth.
Preceptors and clinical instructors who are:
- MGB Employees: full-time, part-time, and Bulfinch Temps are eligible for a 40% reduction in tuition.
- Non-MGB Affiliates: All employees of IHP affiliates will be awarded a 20% reduction in tuition.
We provide preceptors with 104 hours of credit per placement per semester to be used toward their ANCC renewal requirement (i.e., 1 student for 1 day per week per semester provides 104 hours, 1 student 2 days per week per semester provides 208 hours). Once the semester ends, the Office of Clinical Education emails each clinician who precepted that semester a "Certification of Hours for the Semester," certifying 104 credits earned per completed placement.
Our preceptors receive full access to our library of Point-of-Care resources like: Up to Date, DynaMed, National Guideline Clearing House, OvidSP, PubMed@MGH, CINAHL, Cochrane Database of Systematic Reviews, Medline Complete, Clinical Key, and many more.
To request complimentary access, please send the following data points to Joan Parise @ jparise [at] mghihp.edu (subject: Library%20Access%20for%20Preceptors) (jparise[at]mghihp[dot]edu):
- Full Name
- Date of Birth
- Social Security Number
- Email Address
Your request will be promptly processed through our IT department.
Preceptors are eligible to participate in professional development sessions offered by the School of Nursing.
After one year minimum of regular precepting for IHP, preceptors are eligible to apply for adjunct faculty status.
Rank and length of appointment are based on individual applicant’s professional qualifications, length and quality of service to the IHP, such as:
- Precepting service
- Guest lecturer, Term Lecturer for IHP
- Collaborator on scholarly, research projects with IHP
- Leadership partners supporting clinical education of IHP students
- Guest lecturing and teaching opportunities
- Opportunities for collaboration on clinical programs, research