As MGH Institute research portfolio continues to grow, top researchers share what they are working on during Research and Scholarship Day
Research funding at the MGH Institute of Health Professions has increased by an impressive 236% over the past five years, far surpassing the national average for health professions schools.
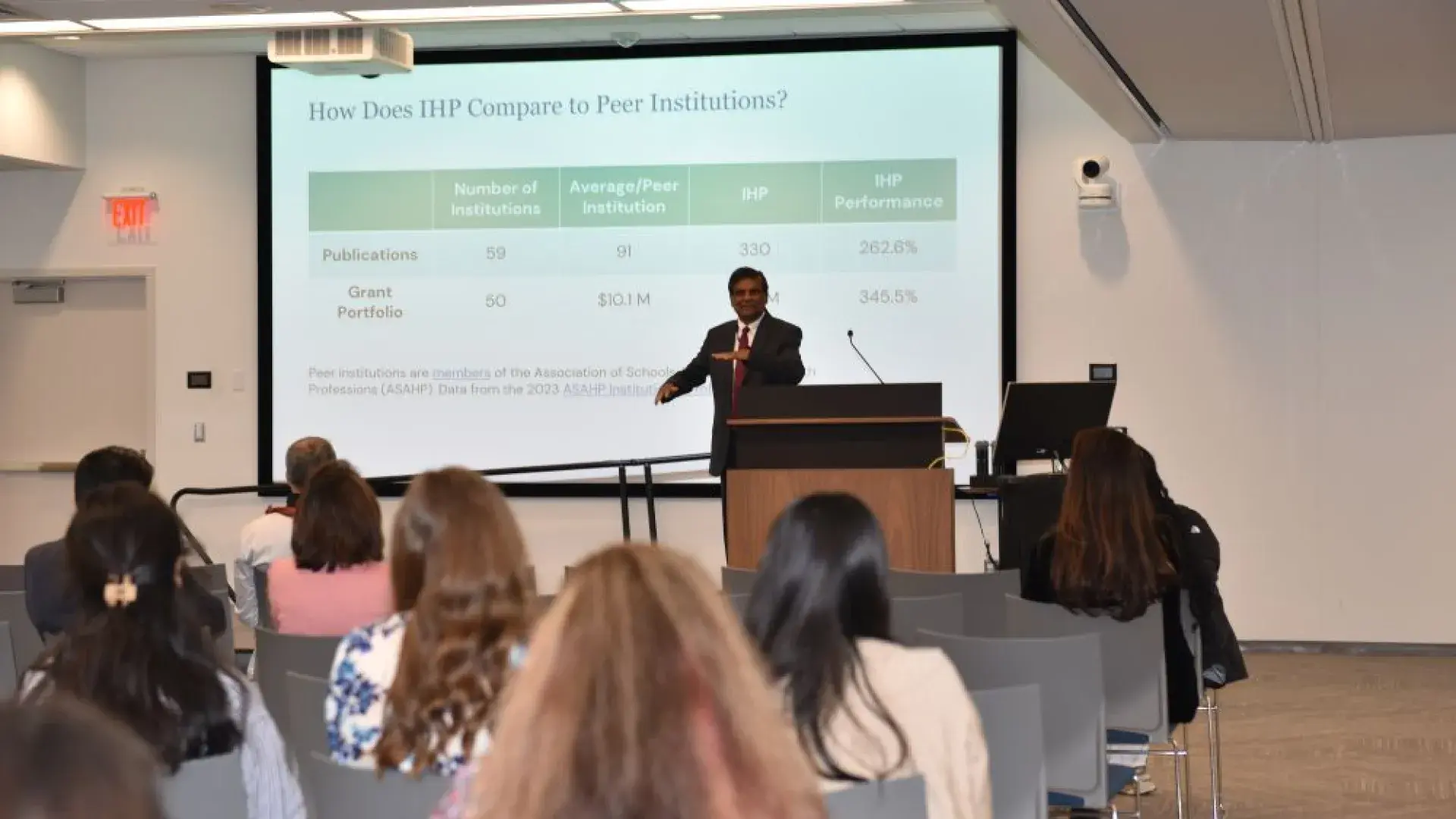
“After all, who wants to be average?” joked Dr. Nara Gavini, associate provost for research, during his opening remarks at Research and Scholarship Day on May 9.
Dr. Gavini addressed attendees in 1CW with a presentation highlighting the Institute’s dramatic research trajectory, from virtually no external funding just a few years ago, to above average by 2020, and now among the leading health professions institutions in grant funding as of 2023.
“There are 59 schools of health professions in the country,” Gavini noted. “The average number of peer-reviewed publications per institution in 2023 was 91. At the MGH Institute, we published 330 papers in the same year. In terms of grant portfolios, only 50 of the 59 schools report any level of external funding. The average is $10.1 million. We were at $45 million in 2023, which is about 305% above the national average.”
Those numbers have continued to rise. According to the most recent figures, the MGH Institute’s grant portfolio exceeded $50 million in the first quarter of this fiscal year. Gavini remains hopeful Trump Administration cuts to the National Institutes of Health funding for research do not affect the Institute’s future portfolio.
The following are highlights from Research and Scholarship Day as several faculty researchers presented their work, underscoring the innovative, interdisciplinary projects that are driving this upward trend.
Brenna Morse and Children with Complex Conditions
Pain is subjective but some children with complex conditions aren’t able to communicate what they are feeling. As a result, those children have greater rates of hospitalization, surgical interventions, disability, and even death compared with the general population of children. Dr. Brenna Morse, now an associate professor of nursing, was working as a school nurse when she became a researcher.
“I was having a hard time finding, evaluating, and knowing what to do when someone came to my office and the teacher said, ‘I think they're not feeling well. I think they have pain,’” said Morse. “So, I studied it.”
In one set of studies, she looked at school nurses, what they said they were doing, and what they were actually doing through analyzing visit records for elementary school children with and without complex conditions who came to the nurse’s office with a headache, stomachache, or sore throat.
“For kids with complex conditions, they were staying in the school nurse’s office for a shorter period of time, so their evaluation was quicker, but they were more likely to stay in the school building,” said Morse. “From this, we knew that kids were possibly in pain, and staying in the care of their school caregivers.
“We wanted nurses, teachers, or specialists in school settings to be prepared to manage pain in this population. I created a workshop that went through the basics of pain, with the neurobiology of pain, and the challenges in this population.”
That work led to focus groups with teachers who spend a lot of time with the children and can differentiate between behavior caused by pain, discomfort, or feeling ill. She also looked at community-based, and hospital-based research to learn as much as possible about caring for kids with complex conditions.
“We learned that it took them an average of a week and a half admission, a lot of clinical tests, specialist consultations, to diagnose them with things like constipation, UTI and ear infection,” said Morse. “Other kids don't have to go to the hospital to get these diagnoses. They don't even always have to go to the doctor to get these diagnoses. Why is it taking us a week and a half to work it up in a kid with complex needs? We wanted to make that shorter more efficient, not only so that kids weren't sitting in pain and suffering, but so their parents didn't have all of the pressures of dealing with it, admission, calling out of work, finding childcare, parking, meals, being in the room. 24/7.”
The next step was developing the Guideline for Ruling Out and Assessing Sources of Pain (GRASP) and building a tool that walks clinicians through presenting symptoms, possible diagnoses to consider and tests to order, which is now in use. It is also being used to train residents as well as parents, to explain what they did, how they ruled out red flags, and why they can take their child home and follow up in a community setting.
At the time of this last study, Morse was working as a home-based complex care nurse and worked to develop a training program for both clinicians and parents. But what she discovered was how important those nurses were to the families and how hard it was to get nurses to work in their homes because of a shortage in Massachusetts.
“There's 850 people who get this home-based complex care,” shared Morse. “They need it to survive and thrive in their own home communities. Those 850 people have three million nursing hours approved each year, collectively and every year, but we have over one million hours unfilled.”
That led to a grant from the state to develop a program to train nurses in home-based complex care. Massachusetts called for training 120 nurses but the MGH Institute helped train 142 nurses and have a wait list of 230 more. The state has extended the grant, and Morse is working to repackage the curriculum and send the program to nursing agencies and every nursing school in Massachusetts.
“It's going to become statewide curriculum. So, every nursing student in Massachusetts can graduate knowing about people with complex conditions, knowing some special considerations for their care, and that working with them in their homes is a career option.”
Prudence Plummer and the Influence of Cognitive Processes on Movement
The act of walking usually doesn’t require a great deal of concentration so there is usually plenty of capacity to do something simple at the same time. But as the combination of the tasks become more complex, there is going to be a change in how well someone can do either of those tasks. That is called dual task interference or a dual task effect. Sometimes, both tasks are affected, which is called mutual interference. Dual-task interference is common after stroke and can create difficulty with everyday activities.
Dr. Prudence Plummer, who directs the Institute’s Cognitive-Motor Behavior Lab and is a Professor in the Department of Physical Therapy, has developed a framework to characterize and classify the types of patterns of interference that occur when someone’s attention capacity doesn’t have enough resources to perform the tasks they are doing.
“Most patients with stroke experience mutual interference when you have them do two things at once,” said Plummer. “But there's also a handful of people who have very little interference on the cognitive task, so they seem to be prioritizing that and mostly having interference on the walking task. So that made me a little curious, why do some people have a mutual pattern of interference, and why do others have a cognitive-priority pattern of motor interference? I've spent quite a bit of time investigating the factors that influence why someone might adopt a certain attentional strategy during dual-task activities.”
The type of cognitive task will impact the dual-task interference pattern and magnitude, with more difficult tasks having more impact. But there are other variables that have an impact, such as the degree of novelty of the task to the person, the enjoyment the person feels from doing the task, and whether a person has the ability to switch their focus from one task to another. People with stroke do not have the same degree of flexibility in allocating attention as healthy adults.
Plummer has studied interventions designed to improve that flexibility performance in people with stroke and other neurological conditions as well as how to predict which patients with stroke will fall during the transition from the hospital to home.
“Failing an attention-demanding task such as stepping over an obstacle might better predict if someone is going to be at risk of falling compared to the simpler clinical measures currently used in the hospital,” she noted.
While it needs validating, the study showed that people who failed an obstacle-crossing test in the hospital before they went home were 10 times more likely to have a fall in the first three months than people who passed the obstacle test before discharge. They also looked at having the people do a step test, which does not permit use of an assistive device, like a walker, to complement the obstacle test and found that it further improved fall prediction accuracy. In new research, Plummer and her team are integrating the use of Apple Watch fall detection and sensor-based technology as well as regular surveys to look at a person’s level of activity, use of assistive devices, fatigue, and other factors, during the first three months after hospital discharge to better understand variables moderating fall risk.
Plummer also shared information on several ongoing projects including a clinical trial combining pharmacological management with rehabilitation for walking impairment treatment in people with multiple sclerosis, looking at the impact of fatigue, and the role of visual attention in cognitive-motor interactions and neurorecovery. Later this month, she will be sharing the results of a study at an MS conference on a collaboration with a medical technology company looking at a novel neuromodulation method for promoting plasticity, the brain’s ability to form new connections, in people with stroke and MS.
Tiffany Hogan and Implementation Science
Dr. Tiffany Hogan, who joined the Institute in 2013 as one of its first researchers, shared how science can serve society through translational research and the work she does to figure out how to close the research to practice gap. It currently takes more than 15 years for less than 15% of research to make it into practice and only 60% of patients with chronic illnesses receive evidence-based care.
“We have a gap in research that’s making it into practice, but we also have a gap between the practice factors that are considered in research,” said Hogan, the Director of the Speech and Language (SAiL) Literacy Lab, and professor in the Department of Communication Sciences and Disorders. “The goal of translational research is to reduce that gap.”
Translational research is characterized into two primary components: implementation science and dissemination science. Hogan focused mostly on her work with implementation science.
“In the past, traditionally, we thought implementation science is more of a linear process. We have to have the evidence first, and then we're going to look at how to implement it,” explained Hogan. “But what we found is that the more contemporary view is that we have to think about clinical practice up front. So, as we're developing the evidence, we want to think about the context in which the evidence will happen.”
One of the examples she shared was hand washing, which is a widely accepted practice in healthcare. But doctors realized hand washing was important well before it was implemented because their environment wasn’t set up to encourage hand washing. Doctors adopted the practice after hand washing stations were set up where they were seeing patients to make it easier for them to wash their hands.
“What works for implementation is to consistently think about a thoughtful plans process, about all the barriers and facilitators at each level,” said Hogan. “We try to think about strategies to eliminate the barriers and enhance the facilitators. Then we put this into practice, and we measure the outcome. Was it done? Did the strategy work to mitigate a specific barrier or not? And then we evaluate it. This is, in a nutshell, the process of implementation science with a goal to create a system that is sustainable.”
Kathy Lyons and Activity Prescriptions
One of the foundational tenets of occupational therapy is that engaging in an activity can change your mood, thoughts, strength, health, identity, sense of time, and well-being. Improvement in these areas is particularly beneficial to cancer patients who may stop doing activities because of symptoms and side effects but even when those things subside, they may not start doing activities again. For 22 years, Dr. Kathy Lyons has been researching activity engagement in people who are living with and beyond cancer, with a focus on increasing activity engagement through activity prescriptions.
“I use the term activity prescription, but it's important to say that in this approach, we don't really do the prescribing,” explains Lyons, a professor at the Department of Occupational Therapy and director of the Cancer Rehabilitation (CaRe) Lab. “It is more of a lifestyle management approach, where we are teaching people to think like therapists and write their own prescriptions for activities that they think are going to increase their health and well-being in the short term.”
The idea is similar to the concept of "personal medicine" developed by Dr. Pat Deegan, a clinical psychologist who works with people with serious mental illness in the recovery movement. Deegan urges people to find their personal medicine — what they do to promote their health — that supplements the medicine that physicians prescribe to treat disease.
To help people establish their activity prescription, the approach gets people to talk about what they want to do that they feel unable to do, why it is important, and why it is challenging. While people point to many things that are related to their cancer treatment, there are many things that keep them from activities that are not related to cancer — feelings of inertia, not feeling as engaged, transportation challenges, weather, etc. — which many people without cancer deal with as well. It may be related to when cancer hits in their lifespan or other things going on in their lives or families.
The OTs using the approach then teach them how to do strategic goal setting — set a goal that's behavioral, observable, achievable, for something they want to do in the next seven days related to this activity. If they know exactly what they want to do, they go right to action planning- describing the who, where, when and how to meet their goal. But often people aren't sure where to start so they are taught to think like therapists and generate options and modify the environment or adapt the activity to make it easier and incorporate those adaptations into their action plan.
Lyons also discussed using this approach in a recent clinical trial on telephone-delivered rehabilitation care. The results, which were published in JAMA Network Open, found that this approach resulted in significantly greater improvements in self-selected activity participation.
“I honestly believe activity engagement is OT’s superpower,” said Lyons as she closed her talk.
Do you have a story the Office of Strategic Communications should know about? If so, let us know.