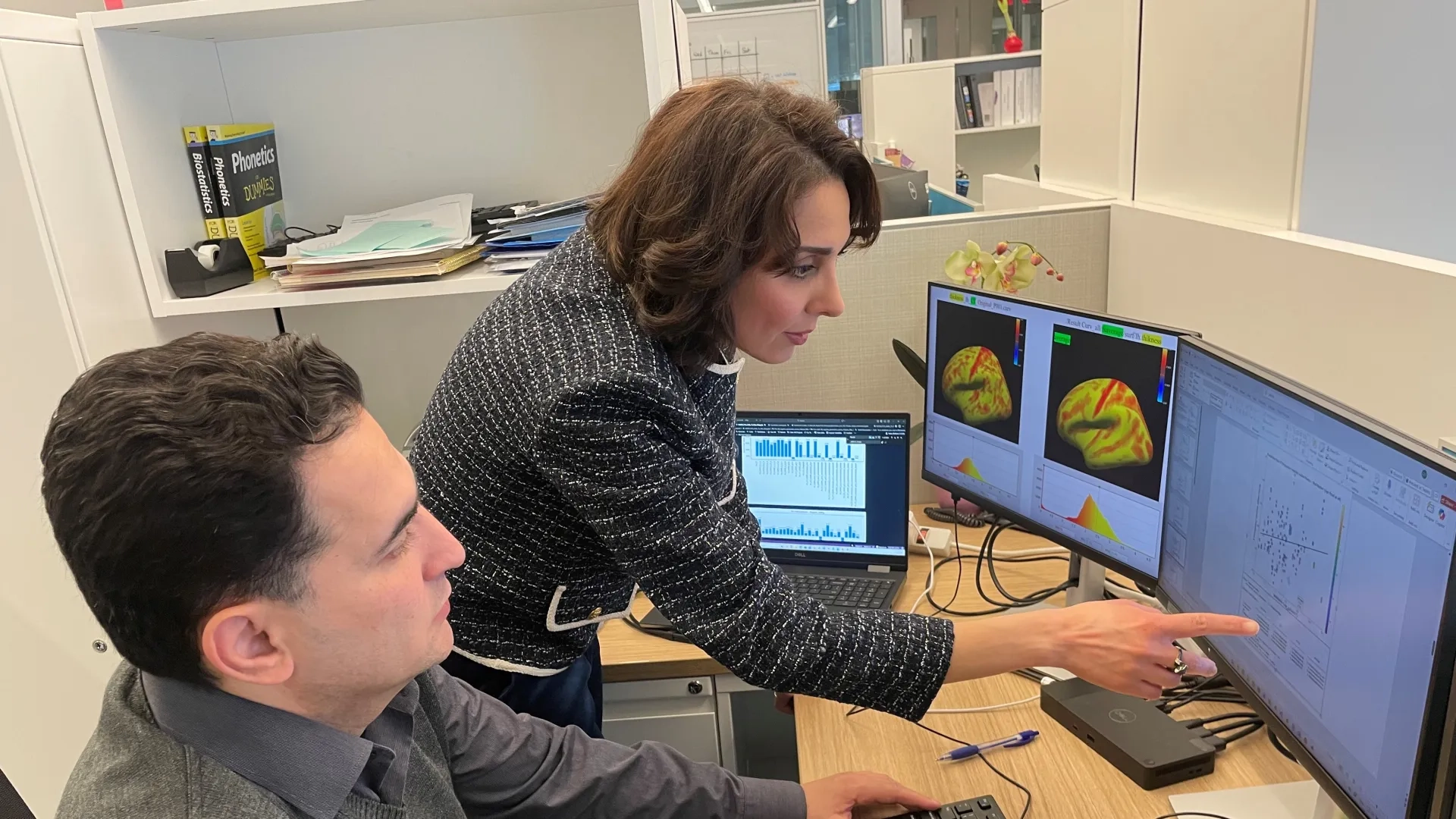
Researcher Marziye Eshghi aims to identify individuals at high risk for Alzheimer’s disease years before clinical symptoms emerge
Can speech and AI revolutionize the way Alzheimer's is diagnosed? MGH Institute of Health Professions researcher Marziye Eshghi, PhD, thinks so, and she’s well on her way to proving it.
“A patient could be within normal limits in the way they speak, but AI could still determine something is wrong,” said Eshghi, Assistant Professor and Director of the Speech, Physiology, and Neurobiology of Aging and Dementia Lab.
Eshghi says her team’s research is distinct in both methodology and scope, integrating speech analysis with genetics, blood-based biomarkers, cardiovascular health, metabolic risk factors such as diabetes, and multimodal measures of brain structure and function, an approach still rare in Alzheimer’s research.
“It's like puzzle pieces that we put together to create a truly holistic picture of what is going on,” noted Eshghi, whose team has spent the past five years analyzing the data they have collected. “Work at this level, across so many modalities, is still uncommon in the field.
“Speech has been overlooked as a biological signal,” said Eshghi. “It’s a remarkably rich behavior, and AI allows us to uncover patterns in natural speech that go beyond human perception and traditional analytic approaches. Our findings demonstrate that speech carries far more information about brain health than we typically recognize.”
Supported by the National Institutes of Health, the ASHFoundation, and the Massachusetts Artificial Intelligence and Technology Collaboratory, Eshghi and her team, working closely with neurologists at Massachusetts General Hospital’s Alzheimer’s Disease Research Center, have spent the past five years exploring how speech acoustic and kinematic properties can reveal early signs of Alzheimer’s disease, often years before traditional clinical methods can detect them. Originally developed for Alzheimer’s disease, this innovative approach is now being extended to other age-related neurodegenerative disorders, including Lewy body disease, Parkinson’s disease, and ALS-FTD, with the goal of uncovering neurobiologically grounded speech features that enhance disease phenotyping and support more personalized clinical care.
Underlying this work is advanced microstructural analysis of speech, powered by artificial intelligence. Eshghi’s team is examining subtle movement and acoustic features that reflect how early molecular pathologies such as tau accumulation, cerebrovascular dysfunction, and APOE‑ε4–related vulnerability affect brain regions responsible for speech motor planning and execution. By quantifying these microscopic deviations, even when speech remains clinically within normal limits, the system can identify individuals who may already be on a path toward Alzheimer’s disease.
“We’ve shown that small departures from typical motor-speech patterns can signal the earliest stages of neurodegeneration,” said Eshghi. “Our AI models integrate speech-derived biomarkers with comprehensive clinical and biological risk profiles, moving us closer to identifying high-risk individuals with precision, before cognitive symptoms emerge.”
While the team’s initial findings are promising, Eshghi and her collaborators are now focused on scaling their research to validate results across larger and more diverse populations. Their goal is to test these models against extensive, longitudinal datasets to ensure robustness and generalizability.
“With expanded data and continued support,” said Eshghi, “we aim to demonstrate that AI models integrating speech-derived biomarkers with comprehensive clinical, biological, and lifestyle risk factors can reliably identify individuals at heightened risk for Alzheimer’s disease well before cognitive symptoms appear.”
A Philosophical Question with Practical Implications
If you could know ten years in advance that you were at risk for Alzheimer’s disease, would you want to know? And if so, what would you do about it?
It’s a deeply philosophical question with profoundly practical consequences. Eshghi’s work aims to give people that very head start: the ability to detect Alzheimer’s-related changes up to a decade before symptoms emerge.
“If an individual understands that they are at higher risk, they can take action, engaging in physical, cognitive, and social activities that have been shown to delay disease progression,” Eshghi explained. Regular exercise, mentally stimulating tasks like puzzles, and maintaining strong social connections all play protective roles. So do a balanced diet, sufficient restorative sleep, and proactive management of cardiovascular and metabolic health, such as blood pressure, cholesterol, and diabetes.
“These daily habits can make a measurable difference,” she added. “They help preserve brain resilience and maintain neural pathways that support memory and executive function.”
While early detection doesn’t erase risk, it empowers people to maximize their cognitive health and quality of life for as long as possible, offering not a cure, but a meaningful extension of vitality and independence.
“This research can make a difference in the lives of so many people,” concluded Eshghi. “A head start to know, followed by lifestyle changes that can help delay symptoms - that combination is a game-changer. That’s why we’re here.”