Hall, Kieran, and Rudolph - who are also Mass General Brigham practitioners - looking to educate and empower nurses through series of journal publications and presentations
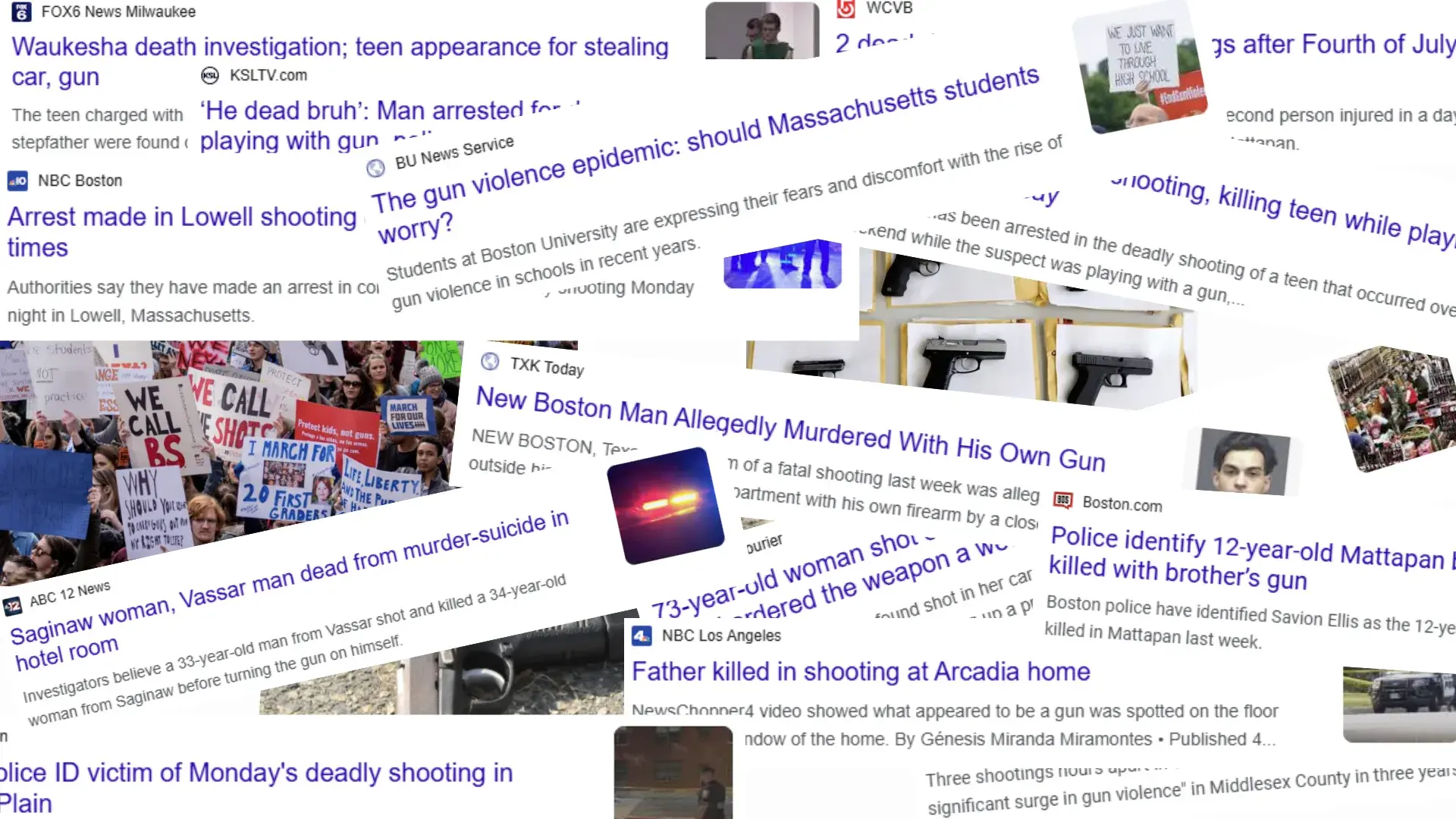
An estimated 132 people in this country will have died today as a result of gun violence. With gun ownership prevalent — 40% of U.S. adults have a gun in the house — the probability of violence or suicide with a gun shows no signs of abating. It begs the question: Is there anyone who can help bring down the rate of gun violence and death?
Nurses, for one.
Three School of Nursing advanced practice faculty, assistant professor Kathy Hall, instructor Kate Kieran, and instructor Meaghan Rudolph, argue that nurses play a significant role in gun violence prevention.
“While we do not have a legal obligation to ask,” said Kathy Hall, an assistant professor of nursing. “Ethically and morally, we do.”
Hall, Kieran, and Rudolph have authored several articles on gun violence; their mission — to educate and empower nurses to take a more active role in learning about guns in the home, offering safe gun storage resources, and having difficult conversations when necessary — all to prevent injuries and death.
“It’s not codified that we have to do it,” said Kieran, who is a mental health nurse practitioner at McLean Hospital. “I've never worked at a hospital where it was a mandated part of the intake assessment, but in mental health, we are strongly encouraged to ask about firearms.”
“From a public health perspective,” said Rudolph, a psychiatric clinical nurse specialist at Massachusetts General Hospital, “just by the statistics, we know this is absolutely a public health crisis.”
In their article, “Gun Violence: What if we don’t ask?” published in the Journal of Legal Nurse Consulting, the trio say research shows that most patients are willing to have assessments of gun storage as part of their care; they warn of consequences if due diligence isn’t conducted.
“Hospitals, healthcare administrators, and healthcare professionals, including nurses,” the authors write, “may face legal consequences if there is a negative outcome related to gun ownership or storage and professionals did not assess for this unique risk that is well established in healthcare literature.”
Hall, Kieran, and Rudolph say nurses are in a unique position to identify risks and mitigate them.
“Asking about firearms in the home is an assessment question that can become as routine as asking about seatbelts, pets, and smoke detectors, not an opportunity for judgment,” the authors state. “Safer firearm storage information is a resource for patients, not a demand for behavior change. Nurses can be effective public safety advocates and protect our most vulnerable patients from firearm violence without offering legal advice, opinions, or political guidance.”
But Hall, Kieran and Rudolph say there are barriers. Nurses do not feel prepared or educated to ask the questions and field the questions from patients or family members. Namely lack of confidence in providing accurate information if there were follow up questions or requests for resources, or even the fear of workplace violence from a patient or family member who takes issue with the line of gun ownership questioning.
While asking about guns may be a simple question, if a patient says yes to guns in the home, the concern among many nurses is: what’s next? Hall and colleagues did a survey of nurses at Massachusetts General Hospital and discovered some worries.
“A lot of nurses felt it was important to ask about gun ownership, but they were concerned about their own safety,” said Hall, a nurse director at Massachusetts General Hospital. “Will the patient become upset by this question? If a patient answers yes that there is a gun in the home, then it’s ‘OK, now what do I do with that information?’ The nurses wanted to know what resources were available to them and to provide patients. Could they give someone a pamphlet on safe gun storage or provide gun locks? So, the response from many nurses was, ‘It's great that I'm assessing this. But then, what do I do with the yes when I get the yes?’”
That’s where a second journal article comes in. “Working Smarter: Facing Firearm Safety,” which has been submitted to the American Nurse Journal. Authored by Kieran, Rudolph, and MGH Institute Associate Professor Brenna Morse, the article discussed that while information about violence, risk, and firearm ownership may surface through conversations, “nurses receive little or no education, training, or support regarding firearm violence discussions and assessing an individual’s risk.”
“Asking about guns in the home as part of a safety assessment is like asking about helmets, seat belts or ungated pools,” they write. “Nurses routinely assess safety and health related risks and provide education on these topics. Nurses can and should engage patients in discussions about gun safety and storage without shame or blame.”
The authors offer guidance on resources that are available, how to coach others to have difficult conversations, and how assess high-risk situations.
“The article is essentially trying to address those concerns,” says Kieran. “It’s a review of ‘Hey, here's why it's important.’ But then also, ‘Here's what you can do, and some reference lists nurses could go to and say, ‘Here's how we talk about it, and here’s some phrases to use.”
The trio sees another barrier in the outpatient settings for advanced practice nurses. Even if they become comfortable asking about guns, the time available during an appointment is limited.
“Often we have so many required assessments to review during a visit,” said Hall. “We need to discuss your blood pressure, lab results, and other important screenings. There are other really important topics, I want to know how you're doing. I want to know what's going on at home. I want to know how work is for you. If you pick up one patient who is at risk by not storing their guns safely and you can educate them, that’s a win.”
Kieran knows all about that. She says the proudest moment in her career was when she convinced a client to relock his guns that he had been leaving around the house. Adding to the risk was an 8-year-old nephew who was visiting.
“I was really proud that we were able to have a family conversation, and he agreed to lock them back up, and I felt like maybe nothing would have happened but what a risk!” recalled Kieran. “We removed that risk after a 10-minute conversation. I think the more nurses also experience that it's not so scary, that people are willing to talk with you, and that you can make a big difference, it’s very rewarding and reinforcing.”
Normalizing conversations about guns comes down to education — early on, say the authors.
“I think one of the best ways to normalize these discussions is to be educating people when they are in training, so it becomes part of their practice,” said Hall. “They just do it.”
Rudolph says the time to establish this kind of questioning is when nurses who are still in training are learning their assessment strategies and developing their skills as well as their standard practices.
“So, if we throw in this added topic once they've already started to get into practice, it’s a bit more difficult,” said Rudolph. “But if we can get this introduced while they're really developing, it'll be infinitely easier to have it flow once they're practicing.”
Publications and presentations are a mainstay for this trio. Hall and Rudolph are contributing authors in the paper, Firearm safety: Nurses’ Knowledge and Comfort published in American Nurse, and Assessing Firearm Access and Providing Safe Gun Storage Education published in MedSurg Nursing, and Nurses' Knowledge and Comfort with Assessing Inpatients' Firearm Access and Providing Education on Safe Gun Storage published in The American Journal of Nursing.
Next month, Hall and Rudolph will present on this topic at the National Organization of Nurse Practitioner Faculties (NONPF) conference in Denver.
While more nurses are beginning to broach the gun conversation, they acknowledge there needs to be more buy-in.
“I think it's progressed, but I don't think it's fully permeated our practice,” observed Hall. “While people realize that it's an important topic to discuss I think we have a way to go to normalize open conversations about safe gun storage, so it no longer feels awkward,” said Hall. “It's just something we do. It's something we ask everybody.”
“It's still seen as niche, and often the job of mental health or the job of someone else,” added Kieran.
If Hall, Kieran, and Rudolph get their way, asking about guns will be the job of every nurse.
Do you have a story the Office of Strategic Communications should know about? If so, let us know.