A grant awarded to physical therapy researcher and professor Dr. Julie Keysor has the potential of giving physical therapists tools to quantify movement during telerehabilitation patient care.
If you’ve ever been to a physical therapy appointment, you’ve experienced someone moving around your leg, shoulder, knee, or foot to measure joint motion and task performance. That physical connection and ability to gather objective clinical measurements is the tried-and-true method of clinical decision making and evidence-based practice.
What happens, however, when physical therapy is delivered through the internet with people in their homes? How can the therapist accurately measure and quantify clinical assessments necessary for decision making and monitoring progress? Thanks to a new augmented reality technology, a TV screen, and a smart phone, a researcher at the MGH Institute of Health Professions may soon have those answers.
A research grant awarded to Dr. Julie Keysor, a professor of physical therapy at the MGH Institute, and Dr. Serge Roy and Bhawna Shiwani from Altec Inc., a research arm of Delsys Inc. and a global leader in sensor technologies. Altec has active research portfolios spanning rehabilitation robotics, speech prosthetics and augmented communication, computer vision (VR/AR telehealth), neural interfaces, and injury prevention. The grant, awarded by the National Institutes of Health’s National Institute on Aging, is a Small Business Innovation Research grant, the first one of which the MGH Institute has ever received.
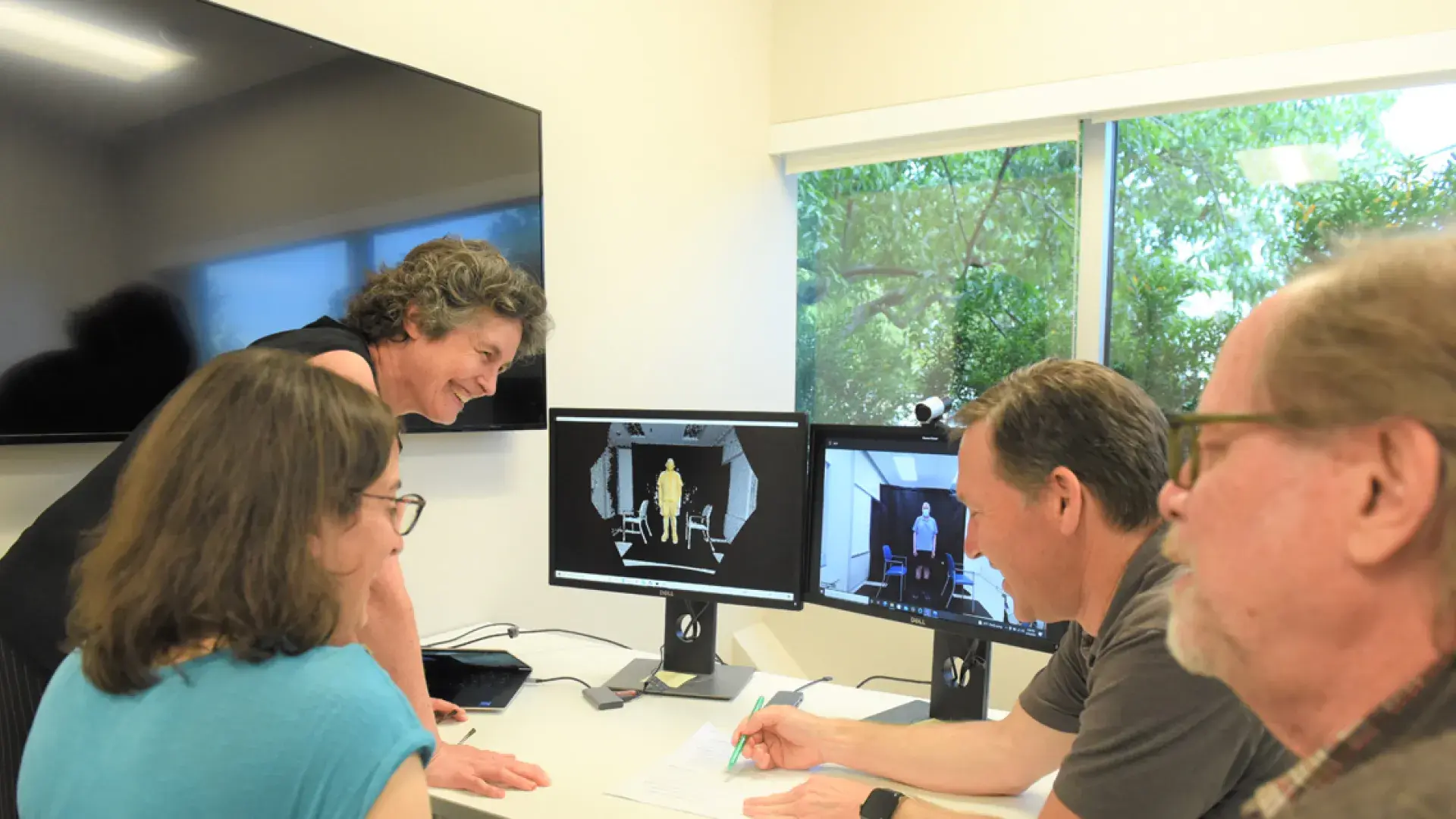
Together, the two collaborative teams will develop a telehealth platform that will allow physical therapists to use video conferencing to measure and quantify joint range of motion, muscle strength, alignment, posture, and how the trunk and upper leg works with the lower leg – tasks that are typically done in-person.
“It could be a game changer, no doubt about it,” said Keysor, who is also Director of the Behavior, Abilities and Technology (B-ABLE) Lab at the MGH Institute. “While there is a little research in using augmented reality for physical therapy treatment, I haven’t seen anyone provide the therapist assessment metrics quantifying movement in real time in the home setting.”
Traditional videoconferencing services allow for a visual check in, but it can’t substitute for in-person physical evaluations currently needed for evaluating joint structure, function, and movement with chronic disabling conditions such as arthritis or recovery from surgical procedures. The ability of a physical therapist to quantify movement is paramount to physical therapy practice.
“It's like a clinician needing to assess a patient who has osteoarthritis and the clinician’s hands are tied behind his or her back because all they can do is look,” said Dr. Roy “Eyeballing it across a video format just doesn't cut it. I've heard people try to put a goniometer on the screen or have the patient take a measurement themselves, but that’s not a very good solution.”
Enter a solution consisting of augmented reality, high-resolution cameras, and custom-designed 3D body tracking algorithms – all of which can be used by a smartphone or tablet to provide physical therapists the quantifiable biomechanical data they need.
“You can't do that in a remote Zoom context right now because there’s no technology that really gives the therapist quantifiable biomechanical information that they really need to guide their clinical decision making and understand how people are progressing,” said Keysor, the primary investigator on the SBIR subcontract. “We want to give the therapist valid biomechanical measures and markers using state-of-the-art technology so they can get the objective measures they need in a remote context.”
This integration of technology can be used at home by patients who interact with a therapist in the clinic. While Keysor and Roy admit it will not replace being in-person, they believe it has the potential to come close.
How It Will Work
Once the app is activated, the patient is guided to make sure they are properly situated in front of the camera, then led through a step-by-step physical assessment specifically built for whatever malady the patient has. For example, if a person has knee osteoarthritis - arthritis in the knee - the app would instruct them to sit, then turn sideways, turn frontward, do a squat – just some of the tasks that make up a pre-programmed sequence of five or six physical activities.
As this occurs, a clinician will watch a real-time video overlay with quantitative measures that will provide quantifiable measurement of, for example, how far a patient can extend and flex their knee.
“The clinician can see, in real time, the starting range and the ending range,” said Roy. “The platform will display the extension and flexing amounts. Those quantifiable metrics would appear as numbers in the corner of the screen.”
The metrics and video, which could automatically become part of patient’s medical records, can provide meaningful information to the medical team as well as the patient.
The app will be tested against sophisticated laboratory equipment; if the two sets of measurements and data match, the research team will know their platform is ready to be reviewed by the Food & Drug Administration – the first step in making it a reality.
Along with Keysor, this research grant also includes four other IHP physical therapy faculty: Assistant Professor Dr. Christopher Clock, Associate Professor Dr. Douglas Gross, Assistant Professor Dr. Rania Karim, and Assistant Professor Dr. Cathy Schmidt.
Possible Uses Down the Road
Keysor and Roy hope the technology can be utilized for both children and adults and include a broad range of conditions such as chronic musculoskeletal conditions like back pain, neuromuscular conditions such as muscular dystrophy, Parkinson’s disease, a stroke, or even recovery from a surgically repaired hip, knee, or shoulder.
“What's most exciting for me about this technology is the ability to link what can happen in the clinic to what is happening in the home for the patient,” said Keysor, who comes to this project with 20 years of arthritis research. “If we can build those bridges, we can really have that clinical care extend into people's home and improve their daily lives.”
This project is being funded by the National Institutes of Health (NIH) – Project # 1R43AG072991-01