IHP faculty lead discussions and showcase innovation in health systems sciences as invited scholars to global forum convened by the National Academies of Sciences, Engineering and Medicine in Washington, D.C.
Ask most people on the IHP campus what Health Systems Science is, and chances are good you’ll get a quizzical look or blank stare. The fact is, most aren’t familiar with the term, but, ironically, the IHP is already a leader in its application to health professions education.
Health systems, like Mass General Brigham, have an increasingly important role in driving innovation in healthcare delivery, research, education, and more. And to improve healthcare and deliver on what experts call the “quadruple aim” - enhancing the patient experience, reducing costs, improving health outcomes, and improving the work life of healthcare professionals - a platform and framework are needed for studying, understanding, and improving how healthcare is delivered.
“Health systems science, or the science of healthcare delivery, aims to understand how healthcare is delivered, how health professionals work together to provide that care, and how the health system can improve care and healthcare delivery,” said Reamer Bushardt, Provost & Vice President for Academic Affairs at the MGH Institute.
The Institute’s leadership in this emerging field was on full display earlier this month during a global forum at the National Academies of Sciences, Engineering, and Medicine in Washington, D.C. There, the IHP presented how it prepares students to apply systems thinking and a health systems science framework during their clinical training experiences, and the Tedy’s Team Center of Excellence in Stroke Recovery was highlighted as an example. Kimberly Erler, Associate Professor of Occupational Therapy, and director of the Tedy’s Team Center of Excellence in Stroke Recovery, presented with Rachel Pittmann, Assistant Dean for Interprofessional Practice, along with several other innovators from across the country. Bushardt moderated the panel discussion, which focused on designing, implementing, and evaluating health system science curricula.
The American Medical Association has done extensive work to advance this emerging field. Medical education has historically involved two pillars—basic and clinical sciences—and the AMA advocates that health systems science should be a third pillar.
“Thinking about health systems science as a new pillar for health professions education makes sense,” said Erler. “There's science happening in the lab that informs our understanding of the human body, injury, and disease. This work is enhanced by clinical science that involves individuals and how we evaluate, prevent, and manage illness. But how do students learn how to bring their knowledge, skills, and abilities together to generate the best outcomes within the spaces where healthcare is delivered? How do students learn to manage the complexity of these environments? The whole idea is that individual encounters between a clinician and the person they are caring for don’t happen in isolation. They occur within systems. And so, we need to better understand how the system impacts people, communities, and health outcomes.”
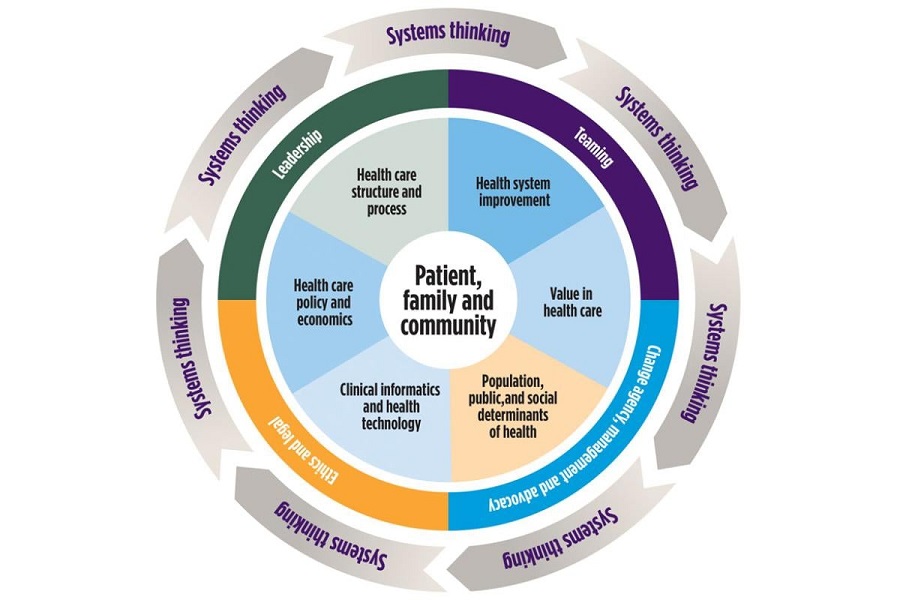
At the center of health systems science are the individuals, families, and communities being served. The health systems science pillar then offers a comprehensive framework of competencies related to value-based care, population health, interprofessional collaboration, health system improvement, and systems thinking. Leading healthcare educational institutions, like the MGH Institute, have found that strengthening core capabilities among its students, such as teamwork and leadership, help them excel in their clinical training and succeed in their careers. The AMA’s framework recognizes those two attributes and highlights other knowledge areas, such as ethics and legal issues, change agency and management, and advocacy. This graphic from the AMA conceptualizes how it works.
Core Functional, Foundational, and Linking Domains for a Health Systems Science Curriculum. The inner circle includes the core functional domains. The middle circle includes the foundational domains. Systems thinking is the domain that links all these concepts together. (Courtesy American Medical Association)
“The American Medical Association has invested heavily over the past decade to promote training in Health Systems Science (HSS) for medical students, residents and practicing physicians, as well as for our colleagues across health professions,” said Dr. Kim Lomis, Vice President, Medical Education Innovations for the American Medical Association. “We see HSS as the third pillar of medical education, alongside foundational biomedical/social sciences and clinical skills. Regardless of how knowledgeable or skilled an individual health professional may be, they will not attain optimal health outcomes for the patients and populations they serve without also knowing how to leverage and navigate the broader health system.”
“The intent is to have everyone in the healthcare system thinking from a systems perspective and being able to think about the interconnectedness of all of its parts,” said Pittmann.
The Tedy’s Team Center of Excellence puts that intent into practice every day. It was created from the observation that the U.S. healthcare system is failing many people in their post-acute rehabilitation, leaving entire populations who need additional services after their insurances ends to reclaim their lives and independence.
“One of the reasons the IHP is ahead of the curve is that our faculty work hard to create authentic learning experiences for students that don’t shy away from the complexity and real-world challenges they’ll face in practice,” shared Bushardt. “It is partnerships like the one with Tedy’s Team, the Spaulding Rehabilitation Network, and the individuals and families who have been impacted by stroke who participate in our program that allow us to create authentic experiences for our students. Under the mentorship of faculty, students help deliver care, learn from those being served, and cultivate systems thinking. Students are strengthening their clinical skills but also gaining insights into healthcare delivery, barriers and challenges faced by families, strategies to improve health outcomes, and advocacy tactics to drive system-level change.”