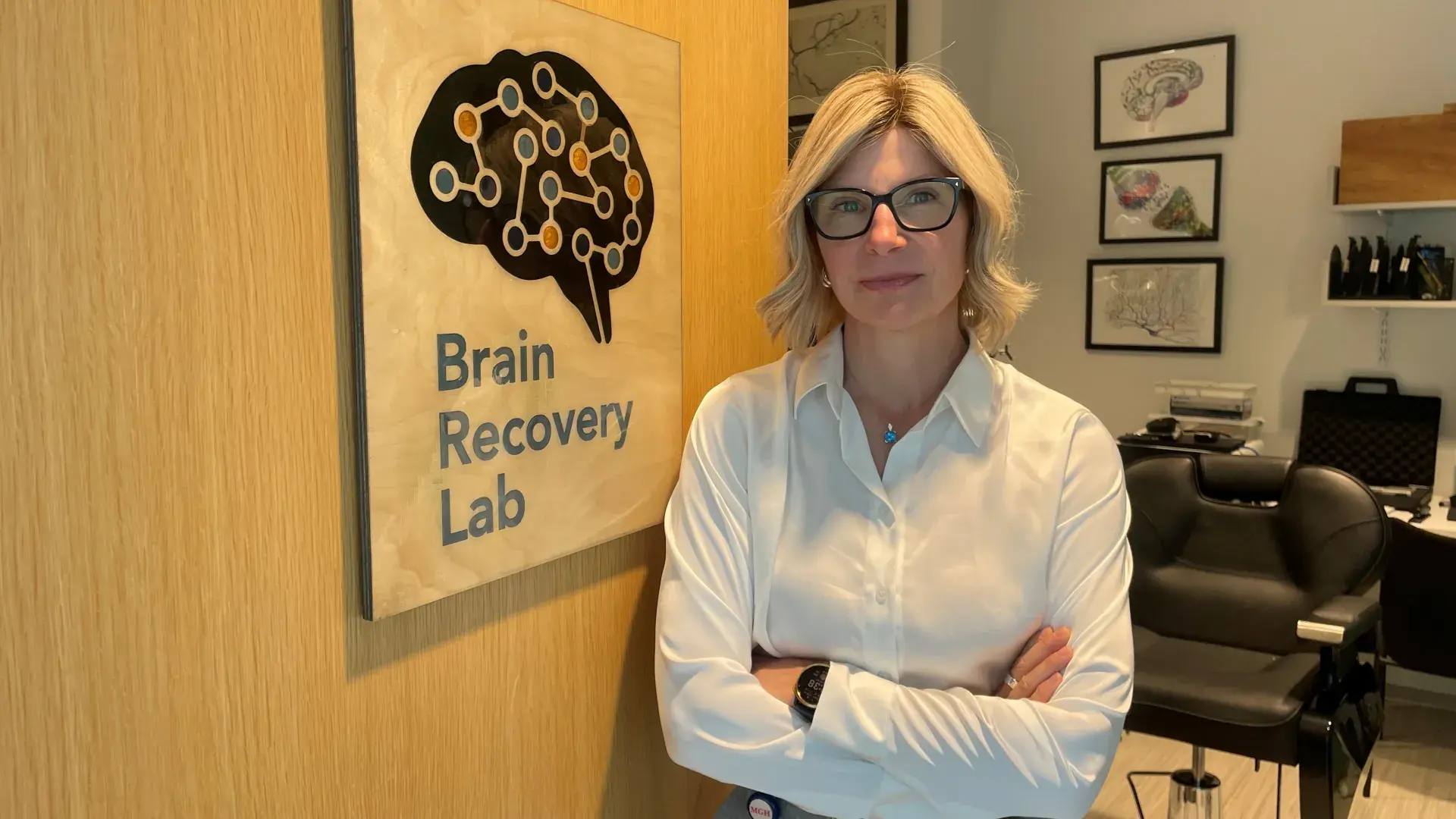
Teresa Kimberley, Director of the MGH Institute’s Brain Recovery Lab, was among the team of stroke experts that helped the American Heart Association (which oversees the American Stroke Association) issue a new policy statement calling for stroke survivors to be discharged based on their functional needs, not their zip code, insurance, or a doctor’s cultural competency. The policy statement was published in Stroke, a peer-reviewed scientific journal.
In this month’s IHP Interview, OSC’s Sean Hennessey spoke with the veteran stroke researcher about the state of stroke recovery, determinants of who receives rehabilitation, and what a better path would be.
You recently helped craft a new policy statement from the American heart Association that says stroke survivors need to be discharged based on their functional needs. Can you expand on that?
Kimberley: In an ideal world, if you have the capacity to participate in three hours of therapy per day after your stroke, you should go to an inpatient rehabilitation hospital, like Spaulding. If you do not have the capacity to do that because you have other medical complications, you might be a better fit for a long-term care facility. Or, if you have a good support network at home, you may discharge to home and access home health or outpatient rehabilitation. Where you go after the acute hospital should be determined by your health and recovery needs.
The best option to achieve maximum recovery after a stroke is most likely inpatient rehabilitation. So, you would assume that our healthcare systems would arrange for the people who qualify to transfer to inpatient rehab. But it turns out that is not the primary factor that determines where people go when they leave the acute care hospital. Numerous studies indicate that a variety of factors besides the care team’s assessment determine where you go. Further, inpatient rehab may not even be presented as an option to you and your family. You, as the stroke survivor or care partner, might not even know that such a thing exists, what the differences in your experience will be, or how that may affect your ultimate recovery.
Studies have shown that other factors are larger influences on whether you are referred to inpatient rehabilitation, such as your geographic region, insurance, or age. If you're older or have a minoritized status, you will be less likely to receive inpatient rehabilitation. It's a huge problem. The factors that are driving where you go after your stroke should be your medical status and capacity to participate in rehabilitation.
What needs to happen in this space for stroke survivors to get better long-term care?
The acute stroke care goal is to save lives, but another important role is to assess the patient’s need and capacity for continued recovery. Acute care rehabilitation professionals (physical, occupational, and speech therapists) should assess patients prior to discharge. Then the whole care team needs to get together to discuss the best option for this person for discharge, based on their medical and recovery needs. The families also need to be educated about what their loved one will receive during the next and important stage of recovery. The difference may be profound - three hours of therapy every day of the week versus somebody coming to your house for 45 minutes once or twice a week. The period of time right after your stroke is vital, as it is when your brain has the best capacity to improve. Short-changing rehabilitation means you may be missing a critical window for recovery, and we don't tell patients about that.
How does that happen that there’s no systematic way to handle stroke survivors the same way?
My guess is that part of the problem is that there isn’t funding for help with transitions in care and there isn’t a mandated framework for the decision and referral process. There needs to be more research to understand what factors predict optimal recovery and response to therapy. Transitions in care is a time-consuming, complex process to do well, and our care teams are already stretched. There is also an issue of access. But if you're at an independent hospital in rural America there may not be a facility with capacity near your family. Throughout the country, there are diverse cultural norms for care after stroke in the sub-acute and chronic stages.
Is funding the common denominator here?
I would say yes. Not all of stroke care is well-funded. Rehabilitation access in general is not reimbursed at high rates, and there are limits to the amount of therapy you can receive, depending on your insurance. With some health insurance plans (ie, Medicare Advantage), you might only get a handful of rehab visits. The system may be incentivized to actually not give you a lot of rehab, even after something as important as a stroke. Often, however, people don't understand this important variable when purchasing plans. Disturbingly, it has been uncovered that some Medicare Advantage providers have systematic processes to deny coverage.
How can long-term stroke care get better?
We need to convince the federal government to understand the benefit of rehabilitation, because then it will be reimbursed at a higher rate, and systems will prioritize rehabilitation. To do that, we need more comparative effectiveness studies that use outcome measures related to the person’s level of function, not just hospital readmission. In some locations, there is a shortage of physical and occupational therapists, so there's a long wait to get in to see them. If hospitals were reimbursed at a higher rate, systems could afford to hire more therapists. For this to happen, we need to have studies that say, ‘If you get this high-quality inpatient rehab, this is where you end up with recovery. And if you don't, this is where you end up.’ These are really hard studies to do, but evidence is needed to change policies. The importance of this issue can’t be overstated. We are talking about a major differential in the quality of your life, your ability to participate in life, the burden that you have on caregivers, and the loss of economic input.
Do you have a story the Office of Strategic Communications should know about? If so, let us know.